Reflections on HIV/AIDS care during my clinical rotations
Introduction
HIV was first correctly diagnosed in the early 1980s in America. From that time onwards, human society has done much to prevent HIV infeciton and mitigate the effects of HIV on the human body. Prevention campaigns have promoted faithfullness in marriage, sex abstinence, condom usage, and more. Highly Active Antiretroviral Therapy (HAART) has been designed to alleviate the effects of HIV on the human body and to prevent eventual progression to the state of AIDS. To date, HIV remains one of the most studied microbial agents. Alot of insights have been garnered on medical management, nursing care, and general prevention and control from this extensive research.
Eternal Stigma
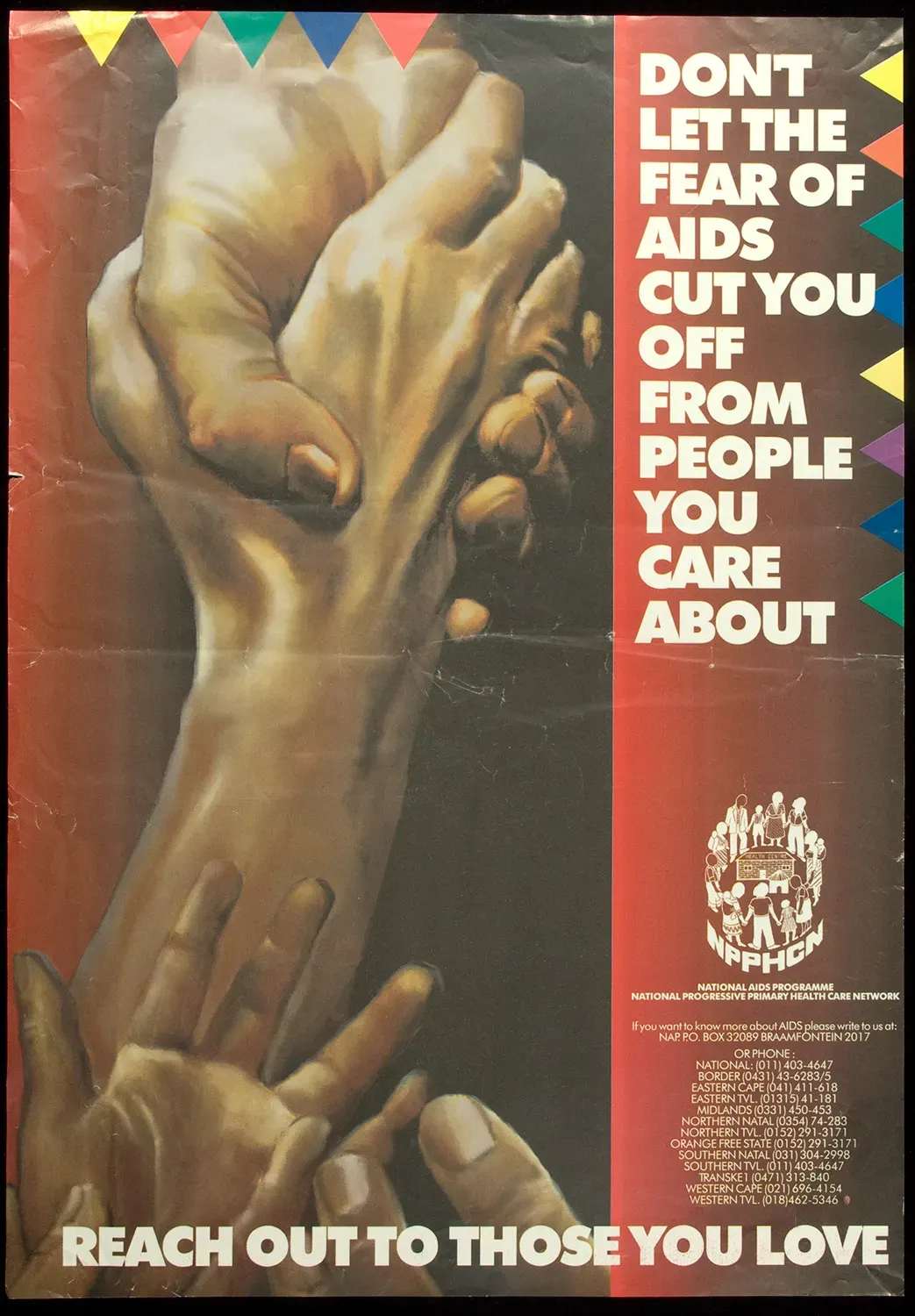
Over the past 4 decades, propaganda and health campaigns spread to the population by governments have been successful in educating the people about basic HIV/AIDS stuff: Prevention and control. That HIV can only be spread by contact with infected persons body fluids either through sex, kissing, or breastfeeding. And yet the stigma associated with HIV is still alive. In hospital wards, patients with HIV face discrimination from everyone in the hospital, from their fellow patients to health care providers. The dread that accompanies HIV infection remains overwhelming.
Personal experiences dealing with HIV/AIDS
During my nursing clinical rotations, I occassionally get the chance to work with HIV and sometimes AIDS patients. On my first clinical rotations, I was completely shocked to learn that a patient I was providing nursing care to was HIV positive. I had never met a HIV positive person. At the moment, a lot of feelings ran through my mind: sudden judgement(this serves you, who told you to go around philandering/hanya'ing), pity for how HIV could have probably ruined his life, and anger that this patient had asked us not to inform his partner about his condition. The patient was most likely progressing to a more advanced stage of HIV infection. Then came the self-directed questions on what I'd do if I were in the patient's shoes. Would i fit in them? . A colleague as if granting me power of attorney, asked that if it were him in a similar condition, I should illegally perform euthanasia on him.
During one treatment session with this client, I have recollections of fluid from his intravenous cannula somehow splashing on my eyes. I had this recollection almost 3 days after the incident. I was very hesitant to talk about this to my colleagues and the nurse in charge. After all, I wasn't sure if it had happened. I also feared the side effects associated with the Post Exposure Prophylaxis drug.
I eventually told my collegues five days after the incident, and I was advised to take a HIV test. I took it and it came out negative. At first I was very anxious about it; I wasn't prepared to live with HIV. It would ruin my life. I never contemplated suicide, however, as I knew HIV can be managed as a chronic disease like diabetes. After three months, I took the same test and it came out -ve again. I was ecstatic for this confirmation.
This experience underscored the importance of understanding PEP protocols and managing anxiety related to occupational exposure risks. Also the prompt reporting the potential exposures.
My second personal experience was with a terminally ill and very symptomatic AIDS patient . Cancerous Kaposi's sarcoma had ravaged both of his feet, and he was no longer able to move. He had what looked like a very bad case of an eye infection on his right eye and had very chronic stages of bedsores from prolonged poor bed positioning prior to his hospitalization. Fungi were growing on his toes. He definitely had serious fungal infections. I asked the nursing in charge what help they were offering the patient and was told that they could not even tell as he was not a patient supposed to be in the ward, and that what they were doing now was palliative care aka end-of-life care. Psychosocial visits were conducted for him. He was off his HAART but surprisingly had shown signs of hope for his future as during the daily wound dressing sessions we'd perform on him, he had shown an interest in the progression of the bedsores wound healing and was very positive about his health. I cant lie to myself, I thought he was going to die in a few weeks.
Confronting my own stigma
For both of these patients whom I was providing primary care for, I felt sympathy, but I could not bring myself to properly work on providing optimal nursing care for them. Absurd as it sounds, I was either constantly anxious about them infecting me overtly by maybe spilling body fluids on me or something or sometimes feeling that maybe the disease was some sort of kamic punishment, that they were paying for all the wrong decisions/actions they had made sometime in their youth. But I was quickly asked by a collegue to consider that maybe they were infected during childbirth. I am still not comfortable working with HIV and AIDS patients as I tend to be very biased when attending to them.
Conclusion
I hope to get over this bias, as the health care provider's main goal is always to alleviate pain and suffering for patients without discrimination. More exposure to diverse population groups and self-reflection are what prove to be essential in developing the empathy and professionalism I will require to provide optimal health care for all patients.
Bibliography
- The New Yorker (2015) Posters from the war on AIDS, The New Yorker. Available at: https://www.newyorker.com/news/news-desk/posters-from-the-war-on-aids (Accessed: 15 September 2024).
- Timeline of the HIV and AIDS epidemic (no date) HIV.gov. Available at: https://www.hiv.gov/hiv-basics/overview/history/hiv-and-aids-timeline (Accessed: 15 September 2024).